What Are The Signs And Symptoms Of Posterior Calcaneal Spur

Overview
If you suffer from heel pain, you know that it affects every step you take. And by the time you take off your shoes in the evening, your feet are really suffering. The pain you?re feeling could be caused by heel bone spurs. Heel bone spurs are common in people who walk, stand or run on hard surfaces such as concrete or tile floors-and that?s most of us! This kind of frequent, intense impact on hard surfaces overstretches and can even tear the ligaments on the bottom of the foot, a condition known as plantar fasciitis. In extreme cases, these ligaments begin to pull away from the bone. Heel bone spurs are created because of this injury to the foot. They are not painful by themselves, but they do irritate surrounding tissues, which causes heel pain.
Causes
Early signs of heel pain are usually due to plantar fasciitis, the inflammation of the plantar fascia. It is probably the most common cause of heel pain seen by the podiatrist. It is seen in all groups of people; runners, athletes, weekend warriors, people who have jobs requiring a fair amount of standing, walking, or lifting, and those who have recently gained weight. The pain most often manifests itself after periods of non-weight bearing when the plantar fascia is given a chance to rest, so your first steps cause a sudden strain to the tissue. Pain is most common with the first steps in the morning and after periods of rest. Fortunately, upwards of 80 percent of those treated early do remarkably well with conservative therapy.

Symptoms
Most bone spurs cause no signs or symptoms. You might not realize you have bone spurs until an X-ray for another condition reveals the growths. In some cases, though, bone spurs can cause pain and loss of motion in your joints.
Diagnosis
Your doctor, when diagnosing and treating this condition will need an x-ray and sometimes a gait analysis to ascertain the exact cause of this condition. If you have pain in the bottom of your foot and you do not have diabetes or a vascular problem, some of the over-the-counter anti-inflammatory products such as Advil or Ibuprofin are helpful in eradicating the pain. Pain creams, such as Neuro-eze, BioFreeze & Boswella Cream can help to relieve pain and help increase circulation.
Non Surgical Treatment
FIRST, Reduce the acute pain. This is done by a combination of several things; injection of a synthetic relative of cortisone into the heel, a prescription of anti-inflammatory pills to reduce inflammation, physical therapy and a special heel pad. About 50% of the time, these treatments will permanently relieve the pain. In the other 50%, the pain becomes recurrent, and the treatment proceeds to Stage II. SECOND, Recurrent, painful heel spur is caused by the tug and pull of the plantar fascia ligament on the heel bone with each step. When the pain is recurrent, arch supports are made to prevent sagging of the arch. The arch supports are custom-made according to the size and shape of the feet. This prevents the arch from sagging and the ligament from tugging and pulling on the heel bone. The inflammation and pain eventually go away as the first phase of treatment is continued along with the arch supports, although the spur itself remains. THIRD, Surgery to remove the spur is possible and is usually done as Day Surgery.
Surgical Treatment
More than 90 percent of people get better with nonsurgical treatments. If conservative treatment fails to treat symptoms of heel spurs after a period of 9 to 12 months, surgery may be necessary to relieve pain and restore mobility. Surgical techniques include release of the plantar fascia, removal of a spur. Pre-surgical tests or exams are required to identify optimal candidates, and it's important to observe post-surgical recommendations concerning rest, ice, compression, elevation of the foot, and when to place weight on the operated foot. In some cases, it may be necessary for patients to use bandages, splints, casts, surgical shoes, crutches, or canes after surgery. Possible complications of heel surgery include nerve pain, recurrent heel pain, permanent numbness of the area, infection, and scarring. In addition, with plantar fascia release, there is risk of instability, foot cramps, stress fracture, and tendinitis.
Bursitis Of The Feet Bursa Treatment
Retrocalcaneal bursitis is sometimes difficult to differentiate from Achilles tendinitis, at least symptomatically. Both are most uncomfortable during the push-off phase of gait, are most severely painful in the morning and with walking after sitting for a period of time, and generally worsen with activity. Most practitioners make the distinction between the two simply on the basis of location of pain and tenderness. Generally, Achilles tendinitis is felt an inch or two higher than this form of bursitis.
Causes
Overuse of the ankle joint may cause irritation of the bursa such as excessive walking, running or jumping. Poor biomechanics and foot function may ultimately lead to heel bursitis due to pulling on the back of the heel by the Achilles tendon.
A sudden increase in physical activity without adequate rest may result in heel bursitis. Excessive standing and walking bare foot on hard surfaces.
Symptoms
Pain at the back of the heel, especially with jumping, hopping, tip-toeing, walking or running uphill or on soft surfaces. If tendonitis is also present, the pain can radiate away from the bursa. Direct pressure on the bursa will exacerbate the pain and should be avoided if possible. Tenderness and swelling which might make it difficult to wear certain shoes on the feet. As the bursa becomes more inflamed you will experience swelling and warmth. In severe cases, the bursa will appear as a bump, called a "pump bump", and is usually red, and extremely tender. Swelling can cause difficulties moving as the range of motion in the ankle can be affected. Limping due to the pain may occur. If you press on both sides of the inflamed heel, there may be a firm spongy feeling. Weakness in the tendons and muscles surrounding the bursa can develop as the pain worsens and the inflammation in the area spreads. Possibly a fever if you are suffering from septic bursitis (You will need to see a doctor for medication to get rid of the infection). Pain at the back of the heel makes it difficult to continue wearing shoes, especially high heels with straps or shoes that don't fit properly.
Diagnosis
When you are experiencing Achilles pain at the back of your heel, a visit to the doctor is always recommended. Getting a proper diagnosis is important so you can treat your condition correctly. A doctor visit is always recommended.
Non Surgical Treatment
With posterior Achilles tendon bursitis, treatment is aimed at reducing the inflammation and adjusting the foot's position in the shoe to relieve pressure and motion on the back of the heel. Foam rubber or felt heel pads can be placed in the shoe to eliminate pressure by elevating the heel. Placing protective gel padding over the painful bursa or stretching the back part of the shoe and placing padding around the inflamed bursa may help. Sometimes a special shoe, such as a running shoe designed to stabilize the midsole heel, devices placed in the shoe (orthoses), or both can help to control abnormal foot and heel motion contributing to the posterior heel irritation. Other shoes have padding that reduces irritation to the posterior heel and Achilles tendon.
Surgical Treatment
Bursectomy is a surgical procedure used to remove an inflamed or infected bursa, which is a fluid-filled sac that reduces friction between tissues of the body. Because retrocalcaneal bursitis can cause chronic inflammation, pain and discomfort, bursectomy may be used as a treatment for the condition when it is persistent and cannot be relived with other treatments. During this procedure, a surgeon makes small incisions so that a camera may be inserted into the joint. This camera is called an arthroscope. Another small incision is made so that surgical instruments can be inserted to remove the inflamed bursa.
Hammer Toe Surgery Foot Problems
hammertoes is a painful deformity wherein a toe bends unnaturally and becomes clawlike. This happens because the tendons of the toe contract abnormally, forcing the toe to bend downward and the middle joint of the toe to protrude upward. Although any toe may be affected, hammertoe usually affects the second toe. The toe assumes a clawlike position and cannot be straightened out. When someone with hammertoe wears shoes, the toe is constantly rubbed, so walking may become especially painful if a callus on the sole of the foot or a corn on the top of a toe develops.
Causes
A hammer toe develops because of an abnormal balance of the muscles in the toes. This abnormal balance causes increased pressures on the tendons and joints of the toe, leading to its contracture. Heredity and trauma can also lead to the formation of a hammer toe. Arthritis is another factor, because the balance around the toe in people with arthritis is disrupted. Wearing shoes that are too tight and cause the toes to squeeze can also cause a hammer toe to form.
 Symptoms
Symptoms
Pain upon pressure at the top of the bent toe from footwear. The formation of corns on the top of the joint. Redness and swelling at the joint contracture. Restricted or painful motion of the toe joint. Pain in the ball of the foot at the base of the affected toe.
Diagnosis
Most health care professionals can diagnose hammertoe simply by examining your toes and feet. X-rays of the feet are not needed to diagnose hammertoe, but they may be useful to look for signs of some types of arthritis (such as rheumatoid arthritis) or other disorders that can cause hammertoe.
Non Surgical Treatment
Apply a commercial, nonmedicated hammertoe pad around the bony prominence of the hammertoe. This will decrease pressure on the area. Wear a shoe with a deep toe box. If the hammertoe becomes inflamed and painful, apply ice packs several times a day to reduce swelling. Avoid heels more than two inches tall. A loose-fitting pair of shoes can also help protect the foot while reducing pressure on the affected toe, making walking a little easier until a visit to your podiatrist can be arranged. It is important to remember that, while this treatment will make the hammertoe feel better, it does not cure the condition. A trip to the podiatric physician?s office will be necessary to repair the toe to allow for normal foot function. Avoid wearing shoes that are too tight or narrow. Children should have their shoes properly fitted on a regular basis, as their feet can often outgrow their shoes rapidly. See your podiatric physician if pain persists.
Surgical Treatment
Surgical correction is needed to bring the toe into a corrected position and increase its function. Correction of the hammer toes is a simple outpatient surgery, with limited downtime. The best option is to fuse the deformed and contracted toe into a straight position. This limits the need for future surgery and deformity return. A new pin that absorbs in the bone or small screw is used by the Foot and Ankle Institute to avoid the need for a metal pin protruding from the toe during recovery. Although the absorbable pin is not for everyone, it is much more comfortable than the pin protruding from the end of the toe. In certain cases, a removal of a small area of bone in the deformity area will decrease pain and limit the need for a surgical waiting period that is found with fusions. Although the toe is not as stable as with a fusion, in certain cases, an arthroplasty is the best hammertoes option.
 Prevention
Prevention
In some cases foot problems may present at birth, many foot problems such as hammer toes can be prevented. Hammer toe prevention can be a simple process, such as, checking your feet regularly and wearing the right shoes for your feet. Good circulation is also an essential part of foot health and hammer toe prevention. Taking a warm foot bath or giving yourself a foot massage are great ways of keeping your feet healthy.
Bunions Foot Pain
Overview
 A bunion is a bony bump that forms on the joint at the base of your big toe. A bunion forms when your big toe pushes against your next toe, forcing the joint of your big toe to get bigger and stick out. The skin over the bunion might be red and sore. Wearing tight, narrow shoes might cause bunions or might make them worse. Bunions can also develop as a result of an inherited structural defect, stress on your foot or a medical condition, such as arthritis. Smaller bunions (bunionettes) also can develop on the joint of your little toes.
A bunion is a bony bump that forms on the joint at the base of your big toe. A bunion forms when your big toe pushes against your next toe, forcing the joint of your big toe to get bigger and stick out. The skin over the bunion might be red and sore. Wearing tight, narrow shoes might cause bunions or might make them worse. Bunions can also develop as a result of an inherited structural defect, stress on your foot or a medical condition, such as arthritis. Smaller bunions (bunionettes) also can develop on the joint of your little toes.
Causes
Bunions have a number of causes, primarily genetics and bad choices in footwear. We inherit traits like flat feet, abnormal bone structure, and loose ligaments and tendons from our parents. When our feet are weakened by these traits and we stuff them into high heels or shoes which don?t support our feet correctly, the repeated stress on the front of the foot may contribute to the formation of a bunion. Other contributing factors are jobs that demand a lot of time standing, obesity, and sudden hormonal changes and weight gain, as in pregnancy. Unfortunately, bunions can lead to many other foot conditions as well. The joint behind the big toe carries much of your body weight and when the bunion makes it sore, you shift your weight onto other areas of the foot. That?s why we frequently see crossover toes, overlapping toes, hammer toes, corns, calluses, and ingrown toenails accompanying bunions. As pain in your foot increases, you?ll also reduce your activity, becoming more sedentary, which has its own quality-of-life issues.
Symptoms
Bunions may or may not cause symptoms. A frequent symptom is foot pain in the involved area when walking or wearing shoes that is relieved by resting. A bunion causes enlargement of the base of the big toe and is usually associated with positioning of the big toe toward the smaller toes. This leads to intermittent or chronic pain at the base of the big toe. Bunions that cause marked pain are often associated with swelling of the soft tissues, redness, and local tenderness. It is important to note that, in post-pubertal men and post-menopausal women, pain at the base of the big toe can be caused by gout and gouty arthritis that is similar to the pain caused by bunions.
Diagnosis
Generally, observation is adequate to diagnose a bunion, as the bump is obvious on the side of the foot or base of the big toe. However, your physician may order X-rays that will show the extent of the deformity of the foot.
Non Surgical Treatment
Nonsurgical treatments such as rest and wearing loose (wider) shoes or sandals can often relieve the irritating pain of bunions. Walking shoes may have some advantages, for example, over high-heeled styles that pressure the sides of the foot. Anti-inflammatory medications, such as acetylsalicylic acid (aspirin, Ecotrin), ibuprofen (Advil, Children's Advil/Motrin, Medipren, Motrin, Nuprin, PediaCare Fever) and naproxen (Anaprox, Naprelan, Naprosyn, Aleve), can help to ease inflammation as well as pain. Local cold-pack application is sometimes helpful as well. To reduce tension on the inner part of the joint of a bunion, stretching exercises are sometimes prescribed. Depending on the structure of the foot and severity of the bunion, custom insole orthotics can slow the progression of the bunion and address underlying biomechanical causes. Inflammation of the joint at the base of the big toe can often be relieved by a local injection of cortisone. Any signs of skin breakdown or infection can require antibiotics. When the measures above are effective in relieving symptoms, patients should avoid irritating the bunion again by optimizing footwear and foot care. 
Surgical Treatment
Larger bunions often require the surgeon to move the entire bone over (1st metatarsal). This is accomplished by a cut or fusion at the bottom of the bone. The former technique, is called the Lapidus bunionectomy. Additionally, the repositioned bone is held in place with one or two surgical screws.
Prevention
Because bunions develop slowly, taking care of your feet during childhood and early adulthood can pay off later in life. Keep track of the shape of your feet as they develop over time, especially if foot problems run in your family. Exercising your feet can strengthen them. Learn to pick up small objects, like a pencil or pebble, with your toes. Wear shoes that fit properly and don't cramp or pinch your toes. Women should avoid shoes with very high heels or pointed toes.
Is Overpronation Of The Foot
One of the most common causes of foot and leg discomfort is a condition known as overpronation. Normal pronation, or "turning inward" of the foot is necessary as the foot adapts to the ground. With over pronation, the arch flattens, collapses, and soft tissues stretch. This causes the joint surfaces to function at unnatural angles to each other. When this happens, joints that should be stable now become very loose and flexible. At first, over pronation may cause fatigue. As the problem gets worse, strain on the muscles, tendons, and ligaments of the foot and lower leg can cause permanent problems and deformities.
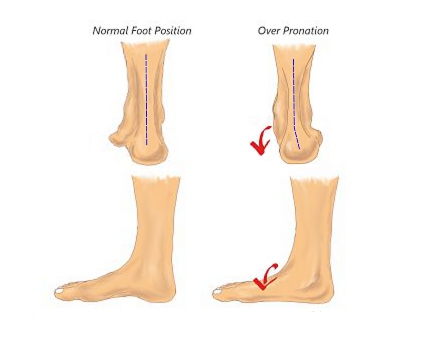
Causes
Overpronation often occurs in people with flat feet, whose plantar fascia ligament is too flexible or too long, and therefore unable to properly support the longitudinal arch of the foot. People tend to inherit the foot structure that leads to overpronation. In a normal foot the bones are arranged so that two arches are formed, the longitudinal and the transverse. Ligaments hold all the bones in their correct positions, and tendons attach muscles to bones. If the bones are held together too loosely, they will tend to move inwards as this is the easiest direction for them to go. Over time the soft tissue structures will adjust to the misalignment and the foot will become permanently over-flexible, with a flat arch.
Symptoms
Common conditions seen with overpronation include heel pain or plantar fasciitis. Achilles tendonopathy. Hallus Valgus and/or bunions. Patellofemoral pain syndrome. Iliotibial band pain syndrome. Low back pain. Shin splints. Stress fractures in the foot or lower leg.
Diagnosis
At some point you may find the pain to much or become frustrated. So what are you options? Chances are your overpronation has led to some type of injury if there's pain. Your best bet is to consult with someone who knows feet. Start with your pediatrist, chiropodist or chiropractor. They'll be able to diagnose and treat the injury and give you more specific direction to better support your feet. One common intervention is a custom foot orthotic. Giving greater structural support than a typical shoe these shoe inserts can dramatically reduce overpronation.
Non Surgical Treatment
If you overpronate, you should talk with a foot and ankle specialist, especially if symptoms have not developed yet. Questions you may want to ask your doctor include what are the best running shoes on the market? Where can I find those shoes? If over-the-counter orthotics don?t work, how long should I wait before contacting you for custom-made orthotics? On my next visit, what type of diagnostic testing should I expect? If I limit the amount of time I spend running, will my overpronation symptoms disappear? What additional treatment options can we try?
Surgical Treatment
The MBA implant is small titanium device that is inserted surgically into a small opening between the bones in the hind-mid foot: the talus (ankle bone) and the calcaneus (heel bone). The implant was developed to help restore the arch by acting as a mechanical block that prevents the foot from rolling-in (pronation). In the medical literature, the success rate for relief of pain is about 65-70%. Unfortunately, about 40% of people require surgical removal of the implant due to pain.
Rehab And Calcaneal Apophysitis
Sever condition is an inflammation of the growth plate of the bone at the back of the heel (apophysitis of the calcaneus). The inflammation of Sever condition is at the point where the Achilles tendon attaches to the back of the heel bone. What causes Sever condition? Sever condition is caused by sprain injury where the Achilles tendon attaches to the calcaneus bone at the back of the heel. Sever condition occurs in adolescent or older children, particularly active boys. It can be very painful. It is one of those conditions commonly referred to as "growing pains." Patients are evaluated for signs of conditions that can mimic Sever condition, such as ankylosing spondylitis and other forms of arthritis. Usually Sever condition is self-limited; that is, it disappears as the child ages.
Causes
The exact cause of Severs disease is not completely understood. It is thought to be associated with an overuse type injury, in which repetitive stress from the Achilles tendon causes a portion of the growth plate to pull away from the heel. In medical terms, this is described as cyclic, micro-avulsion type fractures to the calcaneal apophyses.
Symptoms
The condition can be quite disabling and tends to affect those who are very busy with sporting activities. In the initial stages of the condition, most children displaying signs of Severs disease will tend to hobble or limp off the sports field or court and complain of sore heels near the end of activity. As the condition progresses, children may complain of pain during activity and in severe cases prior to sporting activities. Kids heel pain can be quite discouraging for active children but, early treatment can resolve this type of foot pain in children very quickly.
Diagnosis
Sever?s disease can be diagnosed based on your history and symptoms. Clinically, your physiotherapist will perform a "squeeze test" and some other tests to confirm the diagnosis. Some children suffer Sever?s disease even though they do less exercise than other. This indicates that it is not just training volume that is at play. Foot and leg biomechanics are a predisposing factor. The main factors thought to predispose a child to Sever?s disease include a decrease in ankle dorsiflexion, abnormal hind foot motion eg overpronation or supination, tight calf muscles, excessive weight-bearing activities eg running.
Non Surgical Treatment
Your child's healthcare provider will ask about your child's symptoms and examine your child's feet and heels. Any of the following may be done to treat your child's pain. NSAIDs help decrease swelling and pain or fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If your child takes blood thinner medicine, always ask if NSAIDs are safe for him. Always read the medicine label and follow directions. Do not give these medicines to children under 6 months of age without direction from your child's doctor. Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much your child should take and how often to take it. Follow directions. Acetaminophen can cause liver damage if not taken correctly. Rest will decrease swelling, and keep the heel pain from getting worse. Your child may need to decrease his regular training or exercise. He may need to completely stop running and doing other activities that put pressure on his heel until his heel pain is gone. Ask your child's healthcare provider about activities that do not put pressure on the heel. Ice should be applied on your child's heel for 15 to 20 minutes every hour or as directed. Use an ice pack, or put crushed ice in a plastic bag. Cover it with a towel. Ice helps prevent tissue damage and decreases swelling and pain. Stretching and strengthening exercises may be recommended. A healthcare provider may teach your child exercises to stretch the hamstring and calf muscles and the tendons on the back of the leg. Other exercises will help strengthen the muscles on the front of the lower leg. Your child may be told to stop exercising if he feels any pain. Shoe inserts may be needed. Your child's healthcare provider may give you heel pads or cups for your child's shoes to decrease pressure on the heel bone. You may also be given shoe inserts with firm arch support and a heel lift. Make sure your child wears good quality shoes with padded soles. Your child should not walk barefoot. An elastic wrap or compression stocking may be needed. Your child's healthcare provider may want your child to use a wrap or stocking to help decrease swelling and pain. Ask how to apply the wrap or stocking.
Exercise
Exercises that help to stretch the calf muscles and hamstrings are effective at treating Sever's disease. An exercise known as foot curling, in which the foot is pointed away from the body, then curled toward the body in order to help stretch the muscles, has also proven to be very effective at treating Sever's disease. The curling exercise should be done in sets of 10 or 20 repetitions, and repeated several times throughout the day.
Will Posterior Tibial Tendon Dysfunction (PTTD) Call For Surgical Teatments ?
Overview
Many patients suffer from a ?collapsing arch? or ?flat foot? which can cause pain, instability and difficulty while walking. This condition is more commonly known as Posterior Tibial Tendon Dysfunction (PTTD). PTTD is a progressive flattening of the arch due to loss of function of the Posterior Tibial tendon. As the foot flattens, the tendon will stretch, become insufficient and lose its ability to function. This can have a direct effect on walking and posture, ultimately affecting the ankle, knee and hip. As the condition progresses, the joints in the hind foot may become arthritic and painful. 
Causes
Overuse of the posterior tibial tendon is often the cause of PTTD. In fact, the symptoms usually occur after activities that involve the tendon, such as running, walking, hiking, or climbing stairs.
Symptoms
As different types of flatfoot have different causes, the associated symptoms can be different for different people. Some generalized symptoms are listed. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running and jumping, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time and may experience pain at the inside of the ankle and in the arch of the foot. Feeling like one is ?dragging their foot.? When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain in the bones and tendons in the outside of the ankle joint. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoe wear very difficult. Sometimes, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetic patients may not experience pain if they have damage to their nerves. They may only notice swelling or a large bump on the bottom of the foot. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoe wear is not used.
Diagnosis
The adult acquired flatfoot, secondary to posterior tibial tendon dysfunction, is diagnosed in a number of ways with no single test proven to be totally reliable. The most accurate diagnosis is made by a skilled clinician utilizing observation and hands on evaluation of the foot and ankle. Observation of the foot in a walking examination is most reliable. The affected foot appears more pronated and deformed compared to the unaffected foot. Muscle testing will show a strength deficit. An easy test to perform in the office is the single foot raise. A patient is asked to step with full body weight on the symptomatic foot, keeping the unaffected foot off the ground. The patient is then instructed to "raise up on the tip toes" of the affected foot. If the posterior tibial tendon has been attenuated or ruptured, the patient will be unable to lift the heel off the floor and rise onto the toes. In less severe cases, the patient will be able to rise on the toes, but the heel will not be noted to invert as it normally does when we rise onto the toes. X-rays can be helpful but are not diagnostic of the adult acquired flatfoot. Both feet - the symptomatic and asymptomatic - will demonstrate a flatfoot deformity on x-ray. Careful observation may show a greater severity of deformity on the affected side.
Non surgical Treatment
Initial treatment is based on the degree of deformity and flexibility at initial presentation. Conservative treatment includes orthotics or ankle foot orthoses (AFO) to support the posterior tibial tendon (PT) and the longitudinal arch, anti-inflammatories to help reduce pain and inflammation, activity modification which may include immobilization of the foot and physical therapy to help strengthen and rehabilitate the tendon. 
Surgical Treatment
Flatfoot reconstruction (osteotomy). This is often recommended for flexible flatfoot condition. Flatfoot reconstruction involves cutting and shifting the heel bone into a more neutral position, transferring the tendon used to flex the lesser toes (all but the big toe) to strengthen the posterior tibial tendon, and lengthening the calf muscle. Fusion (also known as triple arthrodesis). Fusion involves fusing, or making stiff, three joints in the back of the foot the subtalar, talonavicular, and calcaneocuboid joints, to realign the foot and give it a more natural shape. Pins or screws hold the area in place until it heals. Fusion is often recommended for a rigid flatfoot deformity or evidence of arthritis. Both of these surgeries can provide excellent pain relief and correction.